Renewing Through The Ny State Of Health Marketplace
You need to renew your Medicaid coverage every year. You can call us at 1-888-432-8026, Monday through Friday, from 8:30 am to 6:00 pm and Saturday 9:00 am to 1:00 pm or visit an enrollment site near you.
The NY State of Health Marketplace will send you a letter or an email with your renewal date for you to call and renew without losing any coverage. Pay close attention to the date on your letter you must renew by that date in order to keep your coverage. You can typically renew 30 days from the date you receive your letter. If you dont understand your letter or if you need help, call us at 1-888-432-8026.
Any information provided on this Website is for informational purposes only. It is not medical advice and should not be substituted for regular consultation with your health care provider. If you have any concerns about your health, please contact your health care provider’s office.
Also, this information is not intended to imply that services or treatments described in the information are covered benefits under your plan. Please refer to your Membership Agreement, Certificate of Coverage, Benefit Summary, or other plan documents for specific information about your benefits coverage.
Back to Top
How To Cancel Medicare Part B
You may be automatically enrolled in Part B medical insurance. When you receive your Medicare card and welcome packet in the mail, the back of your Medicare card will include instructions for disenrolling from Part B.
If you do not initially disenroll in Part B, you will have to do so by contacting your local Social Security office or calling 1-800-772-1213 .
You may not disenroll from Part B online. You will have to speak directly to a Social Security agent to complete the process.
Medicaid Eligibility Rules In The Public Health Emergency
Under Families First Coronavirus Response Act signed on March 18, 2020, establishes a moratorium on Medicaid case closings or reductions. No Medicaid recipient will lose their coverage after March 18, 2020 through the end of the Public Health Emergency. This is part of the “Maintenance of Effort” requirement contained in the Families First law – that gives States extra federal money toward Medicaid costs because of the pandemic.
NEWS: The Public Health Emergency has been repeatedly extended — most recently on These extensions are for 3 months, so the latest one will extend thru July 13, 2022. See this Georgetown Health Policy Institute blog explaining what this latest extension means.
HOW LONG IS THE PUBLIC HEALTH EMERGENCY? The Public Health Emergency has been repeatedly extended — most recently on most recently on See earlier extensions here.
In a bulletin, the federal CMS repeated its earlier promise that states will receive 60 days advance notice before the Public Health Emergency ends, allowing States time to plan for “unwinding” the COVID moratorium on case closings, etc. Under the Trump Administration, the PHE was extended every 3 months, leaving much uncertainty. See this Georgetown Health Policy Institute blog about what the latest extension means.
After the Public Health Emergency is declared over, a process of “unwinding” the Maintenance of Effort protections will begin. On about how this unwinding process will work.
Also Check: Medicaid Services Department Frankfort Ky
Medicaid Enrollees Can Expect To Be:
- Treated with respect and compassion.
- Approved for the most appropriate type of transportation based upon their mobility, medical needs & NYS Department of Health guidelines.
- Served by an on-time, polite & qualified transportation provider.
- Picked up in a safe, clean & smoke-free vehicle.
- Supported by MAS throughout their transportation experience.
Frequently Asked Questions For Current Medicaid Beneficiaries

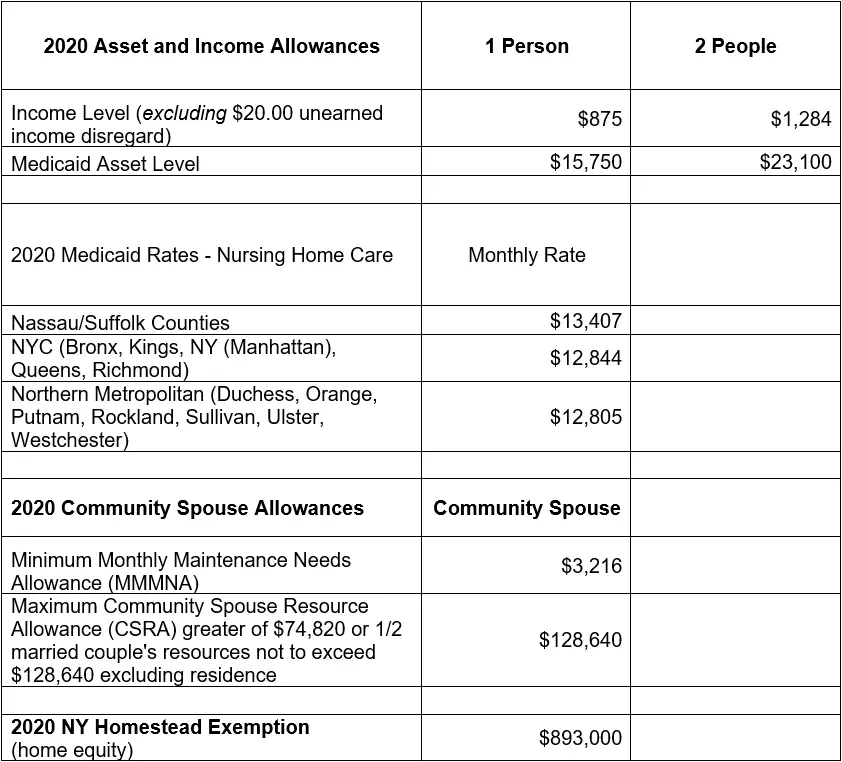
What is a Community Spouse?
A community spouse is someone whose husband/wife is currently institutionalized or living in a nursing home. The community spouse is not currently living in a nursing home and usually resides at the couple´s home.
I am a community spouse. Will I be allowed to keep any income or resources?
If your spouse is institutionalized or living in a nursing home, you will be permitted to keep some income known as a minimum monthly maintenance needs allowance . If you are currently receiving income in excess of the minimum monthly maintenance needs allowance, you may be asked to contribute twenty-five percent of the excess income to the cost of care for the institution
How do I find my local Medicaid office?
The Medicaid office is located in your local department of social services. A listing of offices can be located here:
If you live in the five boroughs of New York City, your offices are run by the Human Resources Administration . A listing of offices can be found here:
How do I order a new benefit card?
If your Medicaid is with your LDSS, to order a new Medicaid Benefit Identification Card, please call or visit your
If your Medicaid is with the and you need to order a new benefit card please call the call center at 1-855-355-5777.
Members residing in the five boroughs of NYC can call the HRA Infoline at 1 557-1399 or the HRA Medicaid Helpline at 1 692-6116.
How often do I have to renew?
You May Like: Can International Students Get Medicaid
How Do I Apply For Medicaid
You can apply for Medicaid in any one of the following ways:
- Write, phone, or go to your .
- In New York City, contact the Human Resources Administration by calling 557-1399.
- Pregnant women and children can apply at many clinics, hospitals, and provider offices. Call your local department of social services to find out where you can apply.
> >
Medicaid In New York State
- COVID-19 News and Updates:
- COVID Information for Medicaid Consumers:
- Medicaid Coverage through Your Local Department of Social Services during the Coronavirus Emergency –
- Medicaid Telehealth Services During the Coronavirus Emergency –
- IRS Form 1095-B Update:
- The 1095-B form for Tax Year 2020 is no longer being mailed automatically.If you need a copy of your 1095-B for Tax Year 2020, you can request it:
- By e-mail – or
Also Check: Paramount Medicaid Ohio Phone Number
How Much Help Someone Gets From Medicaid In New York State Depends On Where They Live
Annie Sibley needs help bathing, getting dressed, cooking meals and cleaning her apartment. A home health aide comes in to help the elderly Syracuse woman with these activities. Without the service, Sibley said she would have to go to a nursing home. Sibley would like to have her aide come every day. But Onondaga County limits her to three two-hour visits a week because the service, known as personal care, is paid for by Medicaid, the government program that covers health care for the needy, the elderly and disabled. If Sibley lived in New York City, she might be able to get approved for up to 24 hours a day of personal care. That’s because many elderly shut-ins get around-the-clock home care in New York City. Medicaid spending on personal care in the Big Apple is more than three times higher per patient than it is in Onondaga County. Some observers see this huge Upstate-Downstate disparity as an area ripe for reform as the state faces a $9 billion budget deficit. Gov. Andrew Cuomo’s administration is looking to save money by overhauling the state’s $53 billion Medicaid program. Gary Fitzgerald, president of the Iroquois Healthcare Alliance, an Upstate hospital trade group, said the cost disparity in the personal care program should be a top priority for Cuomo’s recently appointed Medicaid Redesign Team, charged with finding ways to cut Medicaid spending.
Note to readers: if you purchase something through one of our affiliate links we may earn a commission.
Canceling Magi Medicaid Coverage
Recommended Reading: Blue Cross Complete Medicaid Providers
Canceling Medicaid Managed Care
How To Cancel Medicare Part C
If you wish to cancel your Medicare Part C plan, here is one option for cancelling your coverage:
- The Fall Annual Enrollment Period lasts from each year. During this time, you may disenroll from your Medicare Advantage plan and enroll in a different plan, or you can cancel your Medicare Advantage plan and revert back to Original Medicare coverage.
-
You can take advantage of the Medicare Advantage Open Enrollment Period, which runs each year from .
During this time, you can change from one Medicare Advantage plan to another, whether or not either plan includes prescription drug coverage.
You can also disenroll from your Medicare Advantage plan and switch back to Original Medicare . If you switch back to Original Medicare during this period, you can join a Medicare Part D prescription drug plan.
If you enroll in a Medicare Advantage plan during your Initial Enrollment Period , you can switch to another Medicare Advantage plan or cancel your Medicare Advantage plan and return to Original Medicare at any time during the first three months you have Medicare.
You may be able to cancel your Medicare Advantage plan if you qualify for a Special Enrollment Period .
Recommended Reading: Medicaid Ga Number Customer Service
Canceling Classic Medicaid Coverage
Get Help Switching Or Enrolling In A Medicare Advantage Plan
If you would like further help learning how to cancel your current Medicare coverage for a new Medicare Advantage plan, a licensed insurance agent can help guide you through the process.
Learn more about Medicare Advantage plans in your area and find a plan that fits your coverage needs and your budget.
MedicareAdvantage.com is a website owned and operated by TZ Insurance Solutions LLC. TZ Insurance Solutions LLC and TruBridge, Inc. represent Medicare Advantage Organizations and Prescription Drug Plans having Medicare contracts enrollment in any plan depends upon contract renewal.
The purpose of this communication is the solicitation of insurance. Callers will be directed to a licensed insurance agent with TZ Insurance Solutions LLC, TruBridge, Inc. and/or a third-party partner who can provide more information about Medicare Advantage Plans offered by one or several Medicare-contracted carrier. TZ Insurance Solutions LLC, TruBridge, Inc., and the licensed sales agents that may call you are not connected with or endorsed by the U.S. Government or the federal Medicare program.
Plan availability varies by region and state. For a complete list of available plans, please contact 1-800-MEDICARE , 24 hours a day/7 days a week or consult www.medicare.gov.
Medicare has neither reviewed nor endorsed this information.
Don’t Miss: Trauma Therapist That Accept Medicaid
Unitedhealthcare Senior Care Options Plan
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
American Disabilities Act Notice
In accordance with the requirements of the federal Americans with Disabilities Act of 1990 and Section 504 of the Rehabilitation Act of 1973 , UnitedHealthcare Insurance Company provides full and equal access to covered services and does not discriminate against qualified individuals with disabilities on the basis of disability in its services, programs, or activities.
Also Check: Do Unemployed Qualify For Medicaid
New York State Department Of Health
- Coordinated Care Services, Inc. 613-7673
- Community Services Society of New York 613-7662
You can also visit the New York State of Health website, or call 355-5777 for assistance applying over the phone.
For applicants over 65 years old or disabled, please contact 753-6960 for an application and Supplement A. Applications and Supplement A can also be obtained from the New York State Department of Health.
Unitedhealthcare Connected For Mycare Ohio
UnitedHealthcare Connected® for MyCare Ohio is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees. If you have any problem reading or understanding this or any other UnitedHealthcare Connected® for MyCare Ohio information, please contact our Member Services at from 7 a.m. to 8 p.m. Monday through Friday for help at no cost to you.
Si tiene problemas para leer o comprender esta o cualquier otra documentación de UnitedHealthcare Connected® de MyCare Ohio , comuníquese con nuestro Departamento de Servicio al Cliente para obtener información adicional sin costo para usted al de lunes a viernes de 7 a.m. a 8 p.m. .
You May Like: What Eye Center Accept Medicaid
Withdraw A Fair Hearing Request By Telephone
You may withdraw a request for a fair hearing by calling our statewide toll-free number: 1 209-1134
Speech or Hearing Impaired Individuals
Please contact the New York Relay Service at 711 and request that the operator call us at 1 502-6155. Service at this number will only be provided to callers using TDD equipment.
Supplemental Funeral Assistance Grant
If you are concerned about being able to afford the cost of funeral expenses for a loved one who has passed away, you may be eligible for assistance under the Temporary Assistance program.
The funeral home you are working with can help facilitate scheduling an appointment with our Funeral Assistance coordinator, you may contact her directly at:
Monroe County Office of Faith-Based and Community Initiatives244 S. Plymouth Ave.Rochester, NY 14608 232-3386
Because funeral assistance is a component of the Temporary Assistance program, an in-person interview will be required. Please come prepared to discuss the decedents financial situation, including income and assets. Common income and assets include, but are not limited to, any earned or unearned income due to the decedents estate, life insurance proceeds, social security or veterans death benefits, and bank accounts.
For applicants determined to be eligible for Temporary Assistance, Monroe County will provide a funeral assistance buial grant up to a maximum of $2,500 for decedents aged six years or older, or up to $1250 for deceased children aged five years or younger.
Please note that to be considered a funeral eligible for assistance, the total funeral cost cannot amount to more than $7,000. If the funeral you are arranging will cost more than $7,000, Monroe County will be unable to consider this an indigent burial and we will be unable to provide any assistance.
Don’t Miss: Wellcare Of Ky Medicaid Phone Number
