Emergency Vs Nonemergency Transportation
- Emergency transportation is for the provision of initial, urgent, medical care including the treatment of trauma, burns, and respiratory, circulatory and obstetrical emergencies. Emergency transportation typically emanates from a 911 call.
- Nonemergency transportation necessary in order for an enrollee to access medical care.
Eligibility For The Houston Medical Transporation Program
To receive free rides in Houston to doctors appointments and other healthcare visits, you need to be enrolled in one of these programs:
- Medicaid Medicaid is a program for low-income families and individuals.
- Transporation for Indigent Cancer Patients This service provides transportation to cancer patients with limited financial means from their homes to nearby or distant cancer treatment centers.
- Children with Special Health Care Needs People with cystic fibrosis of any age and children 20 years and younger with special health care needs can benefit from this program.
Volume Of Annual Trips
- New York City 4,800,000 trips
- Long Island 587,000 trips
- Better coordination of services during inclement weather and catastrophes
- Expedited complaint investigation and resolution
- Early identification of transportation access issues
- Increased flexibility and sensitivity to individual enrollee needs
- Improved fraud and abuse identification
Read Also: Does Missouri Medicaid Cover Assisted Living
How Long Will It Take For My Trip To Be Authorized
While most trips can be approved or denied at the time of the phone call, some requests need a longer processing time, such as:
- Appointments to Behavioral Health Services : 5 business days.
- Physical Therapy , Occupational Therapy , Speech Therapy , and Aqua therapy : 5 business days.
- Long Distance Trips: 7 business days.
If you call to request authorization for your trip less than a week in advance, we may not be able to approve your trip.
Transportation Methods Available For Medicaid Recipients In New York
Medicaid is a state and federal program that helps people with limited income and resources cover medical costs .
Though Medicaid readily covers the cost of emergency medical transport for those who are eligible, non-emergency medical transport to medical appointments is a different story.
Non-emergency transportation to and from Medicaid-approved services may be covered, but only with prior approval from a Medicaid caseworker, a ride service, or some other agency.
In this article we will break down how you can get approved for Medicaid transportation in NY and contact information for companies that provide this service.
In New York State medical transportation for Medicaid enrollees who are traveling to receive Medicaid-covered services are managed by two different agencies: Medical Answering Services or MAS and LogistiCare.
MAS and LogistiCare are Medicaid transportation management companies that work closely with medical practitioners as well as transportation providers to make sure Medicaid recipients in New York state receive high-quality, professional transportation services. There are different modes of transportation that a Medicaid recipient might use to go to a medical appointment or to receive some other Medicaid-covered service. These modes of transportation include the following:
â Commercial air
The medical service provider determines which mode of transport is best for the beneficiary based on:
Don’t Miss: How Much Can You Make To Apply For Medicaid
Which Mode Of Transportation Is Necessary
Assessing the most cost effective and medically appropriate mode of transportation.
Medical Justification “2015” Form:
- Requires a medical professional to provide the mobilityrelated reason why the enrollee requires a specific mode of transportation
- Reasons for decreased mobility could be that the enrollee is wheelchairbound, underwent recent surgery to a limb, is blind, or has an unstable gate.
Form 2015
Maintain Original in Medical Record
VERIFICATION OF MEDICAID TRANSPORTATION ABILITIES
Patient Name: _______________________________ Patient Date of Birth __ /__ /____ Patient Medicaid Number: ___________________
Patient Address: ___________________________________________________ Patient Telephone: _______________________________
How To Plan A Ride
Be sure to call at least 24 hours before your doctors visit.
If you are having an emergency, call 911.
Humana Medical Plan members
Humana Long-Term Care Plan members
- Call 1-877-564-0571 to schedule your ride
- Looking for your ride? Call the Where’s My Ride number at 1-866-779-0565
Humana Healthy Horizons in Florida
Don’t Miss: Wellcare Of North Carolina Medicaid
Public Transportation Automated Reimbursement
- NYC
- Medical providers prepurchase Metrocards from the Metropolitan Transportation Authority and distribute them to eligible Medicaid enrollees at the time of appointment.
- The medical provider submits realtime for reimbursement of the MetroCard.
- PTAR reimburses the medical provider $5.50/claim.
To Schedule A Ride Via Fax:
If you are a Medicaid eligible client, Hopelink can offer you an Orca Card as an option to get to your medical appointment.
If you are a Medicaid eligible client, Hopelink can offer you a gas card as an option to cover your costs for getting to and from your medical appointment.
Hopelink can help with reimbursement for parking, bridge tolls, and/or ferry incurred as part of a medical appointment. The Trip Reimbursement Form Letter explains how to complete the form.
The Hopelink Reimbursement Form is to be used when requesting reimbursement for parking, bridge tolls, and/or ferry incurred as part of a medical appointment.
Don’t Miss: Therapist That Accept Medicaid Nyc
Ambulance For Medicaid Recipients
Ambulance services, both ground and air, are an approved mode of non-emergency transportation for certain Medicaid beneficiaries in New York.
The use of an ambulance for non-emergency transport has to be approved through prior authorization by an official who designates whether the ambulance is medically necessary or not. This official will consider whether or not other non-specialized modes of transportation such as a taxi, livery, ambulette, private car, or other forms of public transportation would be more appropriate and perhaps cost effective.
To use an ambulance for non-emergency transportation, the Medicaid recipientâs doctor, physicianâs assistant, or nurse practitioner must order the service on the recipientâs behalf. As a general rule, non-emergency transportation by ambulance is only approved if the Medicaid enrollee is in need of services en route that can only be administered by ambulance.
To procure the use of ambulance for a Medicaid recipient for non-emergency transport, the medical practitioner must reference the patientâs medical records and note the condition that warrants the use of an ambulance. Medical practitioners, programs, or facilities that donât abide by the rules set forth by the state may be sanctioned by the New York State Department of Health.
MTM Transport Services –
â Provides private cars, ambulance, metro and public transit service help, and public bus help and services
From The County To The State
- Prior to 2011 Medicaid transportation was administered by county Departments of Social Services.
- The 201011 State Budget gave the Commissioner of Health the authority to assume the administration of Medicaid transportation from the counties.
- The 2010 Medicaid Administration Reform and subsequent Medicaid Redesign Team initiatives intended to improve the program by:
- Relieving the counties with the burden administering Medicaid transportation
- Improving program quality
- Achieving greater department accountability
- Standardizing the application of Medicaid transportation policy
Read Also: Does Medicare Or Medicaid Pay For Glasses
Well Help You Get A Ride
We will help you get to your doctor visits and the pharmacy. Its easy and free to plan and get a ride:
- You can get a ride to your doctor, the pharmacy, or a healthcare visit.
- You can get as many rides as you need.
- You can plan a one-time ride, or you also can plan rides for regular doctor visits or other appointments.
- Your ride type may be in the form of an independent or volunteer driver picking you up, a ticket for public transit, a taxi, or mileage reimbursement for a friend or family member.
- Your ride type will be based on your needs.
How To Receive Free Gas Money To Get To Your Doctors Appointments In Houston

You will need to call Medicaid Transportation at 877.633.8747 to receive gas money to drive to your doctors appointment.
Medicaid can help you to sign up for the Individuals Transportation Participant Program . In addition, this program can provide gas money to a family member or friend who is willing to give you a ride to your doctor.
Don’t Miss: How Can I Print My Medicaid Card
How Long Does It Take To Get Medicaid In Florida
If you meet the income requirements, you may be able to find out immediately if you qualify for benefits.
However, it usually takes 30-60 days for the application process to be completed.
Once you are approved, it takes approximately 2-3 weeks to get a Medicaid card.
If you need proof of your Medicaid eligibility right away, you can print a temporary card from your MyACCESS Account.
Logisticare Is Now Modivcare Your Benefits Have Not Changed
To help you get healthy and stay healthy, we can provide rides to your medical appointments at no cost to you.
ModivCare provides transportation for Sunshine Health Medicaid members. There are no limits to the number of trips during the year between medical appointments, healthcare facilities or pharmacies.
You May Like: How To Get Medicaid For Seniors
Southeastrans Trip Reservation Line 855
As of June 1, 2018, FSSA began working with a company called Southeastrans to manage all non-emergency transportation for Traditional Medicaid members This includes any member who is NOT in a managed care program such as Hoosier Healthwise, Hoosier Care Connect or the Healthy Indiana Plan. Southeastrans is working to make it easier for these members to find rides to the doctors office, pharmacy or other medical office.
To request a ride, members should first call Southeastrans at 855-325-7586 at least two business days in advance. If your ride is approved, Southeastrans will call you to confirm your ride at least 24 hours before you will be picked up. Rides should only be requested if the member has no other transportation option available.
You can also schedule your rides online using the Southeastrans member portal described below. Please call during regular business hours, Monday Friday, 8 a.m. 6 p.m. EDT. Below are answers to some of the questions you might have.
What does this change mean for me?
Southeastrans provides transportation case management for your Medicaid-covered rides to doctors offices, pharmacies or other health care offices. There is a new number to call to request rides. The Southeastrans Reservation Line, 855-325-7586, is available Monday Friday from 8 a.m. 6 p.m., EDT.
How far in advance do I need to call?
What if I have an emergency?
Emergency transportation needs are not scheduled through Southeastrans call 911.
You will need:
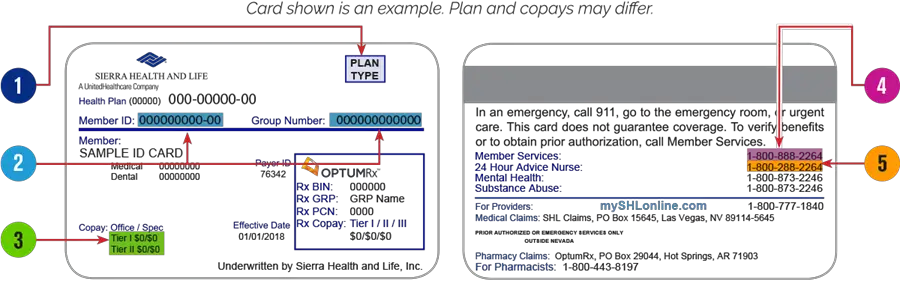
What Information Do I Need To Have When I Call
- Your Medicaid ID number
- Your name
- Information on how you have been getting to your medical appointments before using this service
- If there are medical or non-medical reasons why you cannot use public or other transportation
- The date and time of the appointment
- Your pick-up address and phone number
- The address and phone number where you are going
- The name of the office/clinic/hospital where you are going
- The name of the doctor you will be seeing
- The general reason for your doctors visit
- If you use a walker, wheelchair, or cane
- If you can travel by yourself
- The name of your preferred transportation company
Also Check: How Do I Add My Newborn To My Medicaid
What Is Medicaid Transportation
Medicaid Transportation is a program that offers free transportation for Medicaid patients. This transportation program takes Medicaid patients to medical appointments. This includes free rides to medical appointments in Houston whether its to see your PCP, dentist, or pharmacy.
Editors Note: The official name of this program is called Medical Transporation Program. These free transportation services in Houston, TX are managed by the Texas Health and Human Services Department.
Get Important News & Updates
Sign up for email and/or text notices of Medicaid and other FSSA news, reminders, and other important information. When registering your email, check the category on the drop-down list to receive notices of Medicaid updates check other areas of interest on the drop-down list to receive notices for other types of FSSA updates.
You May Like: Is It Bad To Be On Medicaid
How Do Enrollees Get Transportation
- The medical provider or the enrollee contacts the appropriate transportation manager to request transportation:
- The Department of Health´s policy requires 3 days´ notice for nonurgent trips. Every effort is made to assign trips made with less than 3 days´ notice, as available transportation options decrease as vendors shore up their daily trip rosters.
- Urgent trips and hospital discharges are not subject to the 3day window, and are considered priority.
Mas Can Be Contacted By Calling1
Persons with an active Medicaid case and a medical need and no means of transportation may get help with transportation to and from health care providers .
All non-emergency trips require prior approval and must be requested at least 3 days prior to the date of the trip. Medicaid recipients who provide their own transport should call for information on reimbursement.
The State has contracted with MAS statewide to provide approval and arrangement for Medicaid medical transportation.
MAS can be contacted by calling 1-855-360-3550.
An account will need to be create with MAS to get approval for transportation.
This can be done on the MAS website: www.medanswering.com.
Recommended Reading: Vermont Medicaid Dental Fee Schedule
How Do Medicaid Enrollees Get Transportation
The Medicaid recipientâs medical provider or the recipient must contact a transportation manager at LogistiCare or MAS to make a request for non-emergency transportation services.
The New York State Department of Health requires 3 daysâ notice for non-emergency transportation. Though transportation agencies such as LogistiCare and MAS make every effort to arrange transportation services with less than 3 daysâ notice, transportation options decrease substantially as transportation service providers fill up their daily rosters.
If there is an urgent need for transportation, or if a Medicaid patient is being discharged from the hospital, this request for transportation is considered to be an urgent priority and is not subject to the 3-day advance-notice requirement.
When a Medicaid enrollee calls the transportation manager to request transportation, the manager will ensure that the enrollee has Medicaid coverage and that they are requesting transportation to a location within their service area.
Then, the manager will consider the mode of transportation requested to determine if it is medically necessary and cost effective. The enrolleeâs address and pick-up time as well as the destination address, appointment time, and location within the facility will also be recorded by the manager. Non-urgent transportation to doctors, approved therapists, and dentists are all covered by Medicaid with pre-approval.
How To Schedule A Medicaid Transportation Ride In Houston
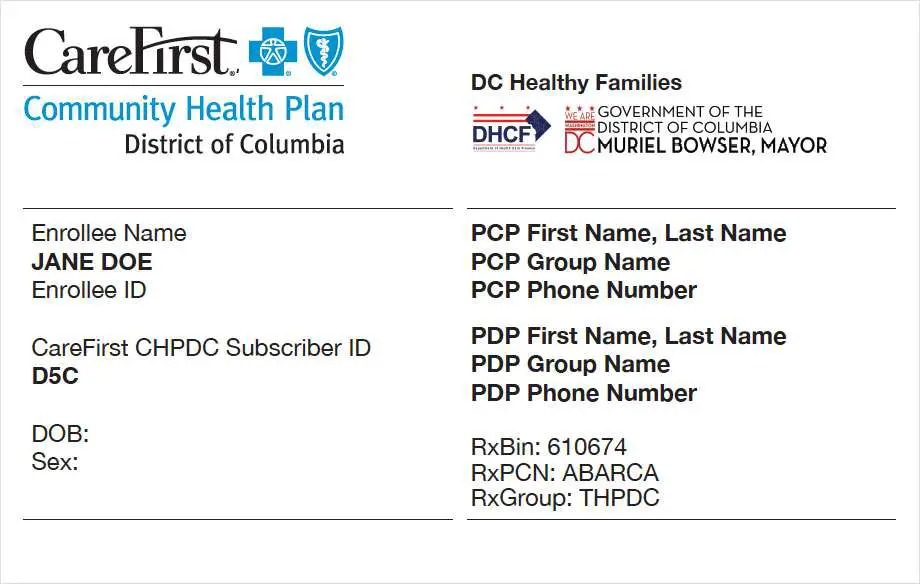
If you have Medicaid and want to schedule a ride through the Medical Transportation Program in Houston you will need to contact the specific insurance company that you have. This means calling the transportation number on the back of your United Healthcare, Molina, or Amerigroup plan to coordinate your free ride to the doctor.
Editors Note: Prior to June 1, 2021, you called a Houston area Medicaid Transportation number to schedule your ride. Now you will need to contact the specific insurance company that you receiver coverage through.
To coordinate your Medicaid transportation ride in Houston, find the specific insurance plan that you have and used the numbers found below to set up your trip.
Don’t Miss: Pediatric Dentist St Louis Medicaid
What If I Cant Find A Transportation Company To Take Me To My Appointment
Occasionally, there may not be a transportation company available in your area that are enrolled in the program or that can take you to your appointment. In that case, we will be unable to assist you with your transportation request. If you have a friend or family member who can transport you to your medical appointments, they may be able to enroll as a private auto provider. They can contact the IMPACT Provider Enrollment Services at 782-5565 or .
How Do I Request Medical Transportation
For complete instructions
You can do it several ways:
Please keep in mind that you may need to call First Transit a few days after you submit to request to check on the status.
Don’t Miss: Does Medicaid Pay For Dentures In Nc
What Is Medicaid In Florida
Medicaid is a federal and state health insurance program for people with a low income.
It provides free or low-cost health coverage to millions of Americans, including families and children, pregnant women, the elderly, and people with disabilities.
The Childrens Health Insurance Program offers health coverage to children in families with incomes too high to qualify for Medicaid, but who cant afford private coverage.
The Medicaid program is different in every state. The federal government sets the general guidelines and each state decides how to run the program.
Florida implemented the Medicaid program on January 1, 1970, to provide medical services to low-income people.
The Florida State Legislature determines who qualifies for Medicaid, what services will be covered, and how much to pay for the services.
The state agency that administers Florida Medicaid is the Agency for Health Care Administration .
