Apply Through The Dutchess County Department Of Community & Family Services If You Are:
- Age 65 and older
- Enrolled in Medicaid Buy-In for Working People with Disabilities enrollees
- Former foster care youth
- Resident of adult homes and nursing homes
- Resident of treatment center/community residences operated by the Office of Mental Health
- Applying for AIDS Health Insurance Program or Medicaid Cancer Treatment Program
- Applying for Medicare Savings Program
- Your eligibility is based on being blind or disabled or you request coverage for community based long term care services including those individuals with an immediate need for Personal Care Services or Consumer Directed Personal Assistance Services
How To Apply For Ny Medicaid
You may apply for Medicaid in the following ways:
- Enrollment Assistors offer free personalized help.
- To speak with the Marketplace Customer Service Center call 355-5777
- Through a Managed Care Organization
- Call the Medicaid Helpline 541-2831
- Through your Local Department of Social Services Office
Where you apply for Medicaid will depend on your category of eligibility. Certain applicants may apply through NY State of Health while others may need to apply through their Local Department of Social Service . No matter where you start, representatives will help make sure you are able to apply in the correct location. For more information on determining your category of eligibility and where you should apply read on.
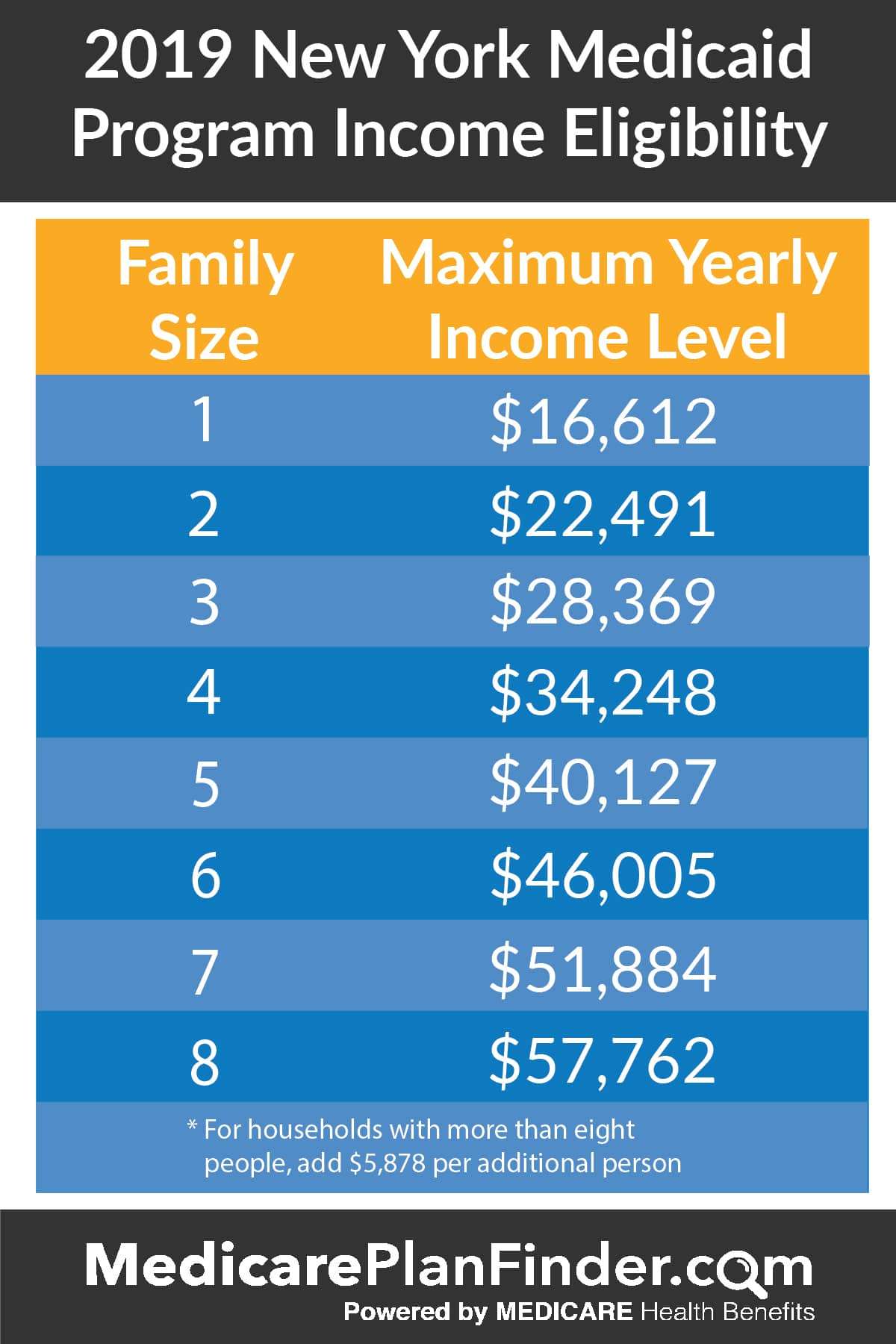
NY State of Health determines eligibility using Modified Adjusted Gross Income Rules. In general, income is counted with the same rules as the Internal Revenue Service with minor variations. Individuals who are part of the MAGI eligibility groups listed below should apply with NY State of Health.
- Adults 19-64 years of age and not eligible for Medicare,
- Children 1 – 18 years of age
- Infants ,
- Pregnant Individuals,
- Parents and Caretaker Relatives of any age
Individuals who are part of the non-MAGI eligibility groups listed below should apply with their Local Department of Social Services .
Other factors that may affect your eligibility include:
- State Residency
- Family or Household size
- Income
Medicaid Application for Non-MAGI Eligibility Group
Supplement A
Does My Insurance Cover Mental Health
Under the Affordable Care Act, all plans purchased through the Health Insurance Marketplace must cover 10 essential health benefits. These include mental health services and substance use disorder services. All Marketplace plans, whether theyre state or federally managed, include coverage for mental health.
Read Also: How Do I Renew Medicaid Online
The Annual Cost Of Aba Therapy
There is no known cure for autism, but there are many treatments that can greatly improve the quality of life for someone on the autism spectrum. These all involve access to health care to some extent, so these treatments are often covered by insurance policies because they are deemed medically necessary.
The specifics of coverage vary from plan to plan. Get to know the specifics of your particular plan to determine the exact level of coverage you can expect for ABA therapy. Even if ABA therapy is covered, you will still have some out-of-pocket costs, such as copays, co-insurance, and deductibles to meet.
The Centers for Disease Control and Prevention estimates that children with autism require an additional $17,000 more per year in care compared to children who are not autistic. Children with severe autism, which can impact motor skills, cognitive function, and verbal communication, may need an additional $21,000 per year compared to their neurotypical peers.
Typical costs involve:
-
Overall health care costs, including regular visits to a pediatrician.
-
Education costs, which may include special education or afterschool programs.
-
Autism-related therapy costs, including ABA therapy, occupational therapy, and speech therapy.
-
Family services, including family therapy.
-
Additional caregivers.
Medicaid Benefits In New York
Medicaid is a state and federally funded program for New York residents who cant afford medical care.
The program provides a number of services, depending on the beneficiarys age, income, and family situation. With over 6.4 million people covered about one-third of the states populationNew York has one of the largest Medicaid programs in the country.
Read on to learn more about New York Medicaid benefits , eligibility requirements, and the application process.
Don’t Miss: Medicaid Fraud Cases In Louisiana
Community And Chronic Medicaid
New York State offers Community and Chronic Medicaid programs for seniors in need of long-term care. While Community Medicaid covers care at home and some assisted living residences, Chronic Medicaid covers nursing home care. Both programs have income and resource limits for eligibility, although the rules are somewhat stricter for Chronic Medicaid.
Does Medicaid Cover All Expenses
Medicaid generally covers all expenses for covered care, but there may be circumstances in which small monthly premiums, deductibles or copayments are required. These include people with incomes above a certain amount in some states or when non-emergency services are administered in an emergency room.
Higher-risk groups such as children and pregnant women are typically exempt from any expenses
Read Also: Where To Find My Medicaid Number
Making The Cost Of Aba Affordable
Costs of a Private Insurance Plan
When getting a private insurance plan, you will owe your monthly premiums to the insurance company and your out of pocket expenses to the company providing ABA services. On a Bronze plan, the premium costs will total $3,050 per year, and the out of pocket costs will likely be $8,550 per year. Before your jaw hits the floor, there are ways to get these costs covered!
Getting Help With the PremiumsThere are autism non-profits that exist to help families cover their premium costs for ABA Therapy. The organization Autism Hero Project is an example of one. Families can complete their quick online application to be considered for a stipend that covers some or all of their premium costs. Applying to such organizations in advance of open enrollment in November can help families secure funding for premiums in advance.
Getting Help With the Out of Pocket CostsCovering premium costs is only one part of the equation. The out of pocket cost is the bigger challenge. Similar to premium cost support, there are also many autism-focused nonprofits that offer grants to families. Autism Speaks has a resource list that can get you started. We have compiled our own grant resource list for families. These are resources that Westside families have successfully used in the past.
Recommended Reading: Pediatric Dentist That Accept Humana Medicaid
How Children With Medicaid Can Access Aba
The most effective path for a family on Medicaid to receive ABA Therapy for their child with autism remains purchasing a private insurance plan during open enrollment. This can be done by connecting with a personal insurance broker. They will help you find an insurance plan.
If you are looking for the best insurance plan to cover ABA, it is likely that the broker will point you to the Blue Cross Blue Shield PPO Bronze Plan. The BCBS Bronze plan has the lowest premium of the BCBS Bronze/Silver/Gold PPO plans. For a single child, the Bronze plan costs $245 per month, whereas the Gold costs $378 per month. More importantly, the Bronze plan has the same exact out of pocket max amount as the other plans .
When you get ABA Therapy, you almost always will meet your plans out of pocket max amount. This amount is likely what you will owe for services for the year. In the case of BCBSs PPO plans, a year of ABA would likely cost $8,550 whether you are on the Bronze, Silver, or Gold plans. If you get the same services for the same cost no matter the plan, it would make sense to buy the one with the lowest monthly premium amount: the Bronze Plan. If you are looking to get an insurance plan for ABA, and someone is recommending the Silver or Gold plan, this should raise questions. It is possible you will be overpaying for the same exact service.
Recommended Reading: Dentist In Lafayette La That Accept Medicaid For Adults
Recommended Reading: Dentist Who Accept Medicaid For Braces
Who Can Get Medicaid In New York
You should apply for Medicaid if your income is low and you match one of the descriptions below:
- You think you are pregnant
- The parent or caretaker of a child and/or teenager under the age of 19.
- You are a child or teenager age 18 or under.
- An adult age 65 or older.
- You are legally blind.
- Living with a disability or disabled.
- You are in need of nursing home care.
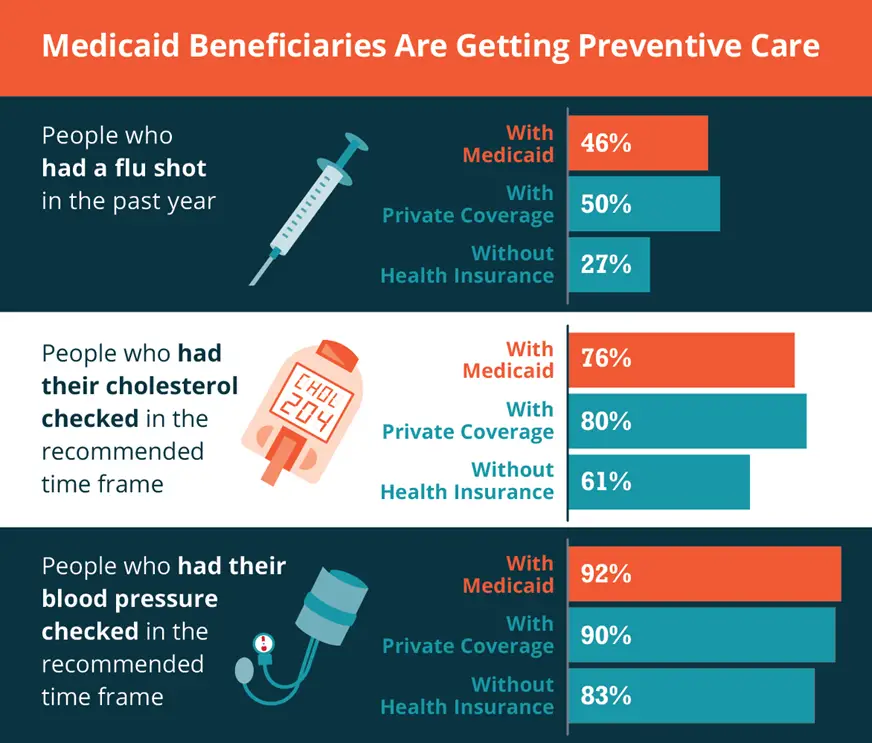
Medicaid Consumer Fact Sheets Now Available
Following a recommendation from the Medicaid Redesign Team II, the New York State Department of Health Office of Health Insurance Programs created Medicaid consumer fact sheets focused on chronic health conditions. Each fact sheet provides information regarding how a condition can be prevented or managed, as well as relevant Medicaid benefits that can be used to help members stay healthy. Topics include sickle cell disease, diabetes, high blood pressure, asthma control, HIV-PrEP , and smoking cessation. Fact sheets can be found on the MRT II Policies and Guidance web page and are available in English, Spanish, Traditional Chinese, Russian, Haitian Creole, Bengali, and Korean. The most recently added Sickle Cell Disease fact sheet is also available in Simplified Chinese, Polish, Yiddish, Arabic, and Italian.
Read Also: Does Medicaid Pay For Over The Counter Medicine
Also Check: Will Medicaid Pay For Assisted Living In Florida
Who Requires A Dental Crown
Since we previously said that crowns are most of the time required and therefore covered by Medicaid, we will discuss a few instances where a crown must be fitted:
- To aid in the protection of a weaker tooth that is about to break or is already damaged
- To aid in the restoration of a fractured or worn-down tooth
- To keep your prosthesis in a place as a bridge
- To conceal discolored or damaged teeth
Your dentist can advise that all of the aforementioned scenarios are medically required. In some circumstances, you will either be fully covered by Medicaid or will be required to pay a co-payment, depending on your state of residency.
What Can I Do To Reduce Taxpayer Funding Of Abortions
You May Like: Does Prenatal Medicaid Cover Dental
Would These Abortions Go Away Without Medicaid Funding
Some would, though some would be paid for privately. When Medicaid does not cover abortions, studies have found that the number of abortions drops by about one-third. Those pregnancies are carried to term, and the child is left alive. Decades of other research on the issue have had similar findings. According to these studies, about a third of Medicaid-funded abortions dont happen if they have to be paid for privately.
In addition, without Medicaid funding, unwanted births decrease as well. Research has shown that when abortion is more difficult to access financially, people take greater care to avoid pregnancy. In fact, the effect is so significant that some studies have found that the number of births actually decreases along with drops in abortions.
Find A $0 Premium Medicare Advantage Plan Today
For California residents, CA-Do Not Sell My Personal Info, .
MedicareAdvantage.com is a website owned and operated by TZ Insurance Solutions LLC. TZ Insurance Solutions LLC and TruBridge, Inc. represent Medicare Advantage Organizations and Prescription Drug Plans having Medicare contracts enrollment in any plan depends upon contract renewal.
The purpose of this communication is the solicitation of insurance. Callers will be directed to a licensed insurance agent with TZ Insurance Solutions LLC, TruBridge, Inc. and/or a third-party partner who can provide more information about Medicare Advantage Plans offered by one or several Medicare-contracted carrier. TZ Insurance Solutions LLC, TruBridge, Inc., and the licensed sales agents that may call you are not connected with or endorsed by the U.S. Government or the federal Medicare program.
Plan availability varies by region and state. For a complete list of available plans, please contact 1-800-MEDICARE , 24 hours a day/7 days a week or consult www.medicare.gov.
Medicare has neither reviewed nor endorsed this information.
Read Also: Best Way To Apply For Medicaid
How Much Do Therapy Sessions Cost
The average cost of therapy is $60 to $120 per session, with most Americans paying between $20 to $250 per hour depending on the number of sessions booked, and if its covered by health insurance. With health insurance coverage, rates average $20 to $50 per session, or about equal to your current copay.
Medicaid Coverage And Aba Therapy For The Treatment Of Autism
There is often nothing about how an individual with ASD looks that distinguishes them from people without an ASD diagnosis. People with ASD, however, may communicate, interact, behave, and learn in ways that are drastically different from most other people. The learning, thinking, and problem-solving abilities of people with ASD can range from gifted to severely challenged. Some people with ASD require significant help in their daily lives others need less.
Recommended Reading: Does Kelsey Seybold Accept Medicaid
News Flash September 201:
In August, 2018, The Legal Aid Society and Willkie Farr & Gallagher filed Ciaramella v. Zucker to challenge the New York State Department of Healths rules preventing Medicaid coverage for replacement dentures within 8 years from initial placement and the ban on Medicaid coverage for dental implants. See article in New York Times, August 2, 2018, “Lack of Dental Coverage Hampers Medicaid Recipients, Suit Says.” In response, DOH will be implementing changes to the dental manual to cover dental implants when medically necessary and to change the rules for replacement dentures. These changes, described below and in this document, will take effect on November 12, 2018. The new rule on replacement dentures imposes new documentation requirements and will be a step backward for some.
Legal Aid Society asks you to let them know if you are working with Medicaid-eligible individuals who require dental implants or replacement dentures, including those whose care may not be covered based on the revised policy. They also want to speak with Medicaid-eligible individuals who require any other dental treatments that are not covered by Medicaid including root canals, immediate dentures, osseous surgery. Contact: Legal Aid Society Health Hotline 577-3575 or .
WHAT DENTAL SERVICES ARE COVERED UNDER MEDICAID?
Benefits Covered For All Of Our Medicaid Managed Care Members
Learn what the plan offers and how it can benefit you.
Preventive care helps prevent health problems and find them before they get serious. Includes routine and sick visits to your primary care physician and other network providers for:
- Regular checkups
- Well-baby and well-child care
- Eye and hearing exams
- Eyeglasses and other medically needed vision aids
- Regular gynecological exams
- HIV counseling and testing services
- Smoking cessation counseling
- Four fluoride varnish applications
When medically needed, your doctor will refer you for:
- Lab work
- Medically necessary abortions
- Screening for anemia, cervical cancer, sexually transmitted diseases, hypertension, breast disease, pelvic abnormality and pregnancy
You can get these services from EmblemHealth network OB/GYN doctors. Or, you can use your Medicaid card if you want to go to doctors or clinics out of our network. Either way, no approval or referral from an EmblemHealth network doctor is needed to get these services. Just make an appointment.
Recommended Reading: Medicaid Out Of Country 30 Days
Elective Benefits State By State
Many states elect to offer benefits outside of the ones listed above, completely or partially. A few examples of elective benefits are visits to specialists, prescription items, vision care, dental care, and some screening services. All of these and others will be covered in some states but not in others.
The rest of the article will outline each states elective benefits. To learn all of the benefits offered by Medicaid in your state, be sure to include the above mandatory benefits with all of the benefits listed below by your state of residence.
| Alaska |
What Is Monaural Hearing Aid
The word âmonauralâ refers to sound reception in one ear only. A patient with âmonaural hearing lossâ has hearing loss in just one ear. A monaural hearing aid is a device thatâs worn in just one ear to correct a patientâs hearing. Monaural hearing aids were once the standard. Indeed, as recently as 1984, about 78% of all patients who had hearing aids had monaural fittings. Some recent studies have shown that patients with monaural fittings experienced hearing loss in the ear that was not wearing a hearing aid. This is called the Monaural Hearing Aid Effect. But while some studies support the use of binaural hearing aids even for monaural hearing loss, other studies have shown that patients with hearing loss in both ears experience no statistically significant difference in terms of their hearing quality whether they use monaural or binaural hearing aids to correct the problem.
The patientâs otolaryngologist or audiologist will likely recommend the best hearing aid that will conform to the necessary specifications to guarantee coverage by Medicaid in New York. Patients must then decide whether the prescribed hearing aid provides substantial hearing and health benefits or not.
You May Like: First Choice Medicaid Sc Address
