Medicare Dual Eligible Special Needs Plans
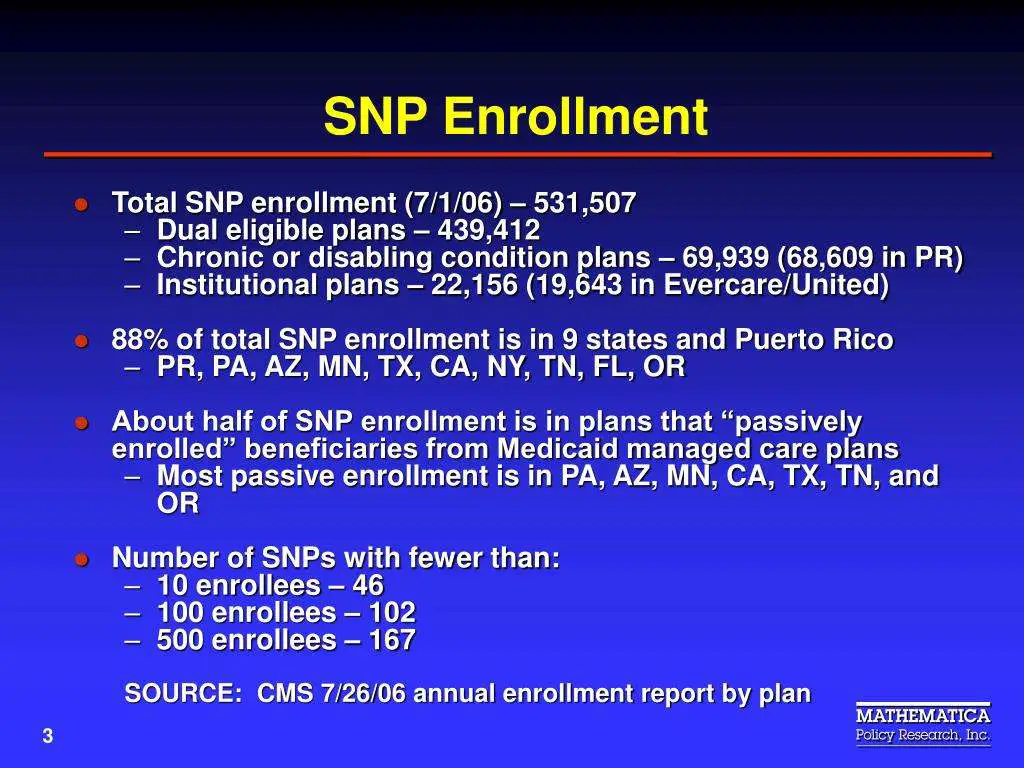
Another type of coverage that may be available to dual eligible beneficiaries is a Medicare Dual Eligible Special Needs Plan .
A Medicare special needs plan is a certain type of Medicare Advantage plan that is designed for people with specific health conditions or circumstances.
A D-SNP is built for the specific needs of dual eligibles. All Medicare SNPs provide prescription drug coverage.
Unitedhealthcare Dual Complete Plans
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. This information is not a complete description of benefits. Call TTY 711 for more information. Limitations, co-payments, and restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
American Disabilities Act Notice
In accordance with the requirements of the federal Americans with Disabilities Act of 1990 and Section 504 of the Rehabilitation Act of 1973 , UnitedHealthcare Insurance Company provides full and equal access to covered services and does not discriminate against qualified individuals with disabilities on the basis of disability in its services, programs, or activities.
You May Like: Dentist That Accept Medicare Medicaid
Who Is Dual Eligible For Medicare And Medicaid
To be Medicare dual eligible, you have to meet the requirements for Medicare and your states Medicaid program.
To be eligible for Medicare, you must:
- Be at least 65 years old or having a qualifying disability
- Be a U.S. citizen or permanent legal resident
- Be eligible for benefits through Social Security or the Railroad Retirement Board
Generally speaking, Medicaid provides health insurance to low-income individuals and families, children and pregnant women. The best way to find out if you are eligible for Medicaid is to visit your states Medicaid website.
If you’re eligible for Medicaid and want to find out if you’re also eligible for a dual-eligible Medicare Medicaid plan, you can all to speak with a licensed insurance to find out if you’re eligible. An agent can help you compare the plans that are available where you live and find out what they may cover, which could include benefits like prescription drugs and other services.
Find $0 premium Medicare plans in your area
Or call 1-800-557-6059TTY Users: 711 24/7 to speak with a licensed insurance agent.
Dual Special Needs Plans In 2022
Californians on a UnitedHealthcare Dual Special Needs Plan get many extra benefits beyond those you get with either Original Medicare or Medi-Cal.
- $0 drug copays on all tiers of covered medications with option for home delivery
- Up to $1,500 for covered types of preventive and comprehensive dental services
- Up to $600 per year to buy over-the-counter products for home delivery
Read Also: Find A Neurologist That Takes Medicaid
Distinguishing Between Medicare And Medicaid
Applicants qualified for both Medicare and Medicaid programs are referred to as Medicare-Medicaid enrollees having dual eligibility. Since the terms Medicare and Medicaid can be easily confused, it is essential to distinguish between them. While Medicare coverage is a federal health insurance program for seniors and people with disabilities, Medicaid is a state and public medical assistance program for people of all ages who need financial support. Both programs provide several benefits, such as doctor visits and hospitalization, but only Medicaid offers long-term nursing care. Particularly relevant to the subject of this article, Medicaid also covers long-term care and supports in-home and community-based settings, such as ones own home, an adult foster care residence, or an assisted living facility. However, beginning in 2019, Medicare Advantage plans began providing some long-term home and area-based benefits.
The CMS is in charge of both the Medicare and Medicaid programs. CMS collaborates with state agencies to administer the Medicaid program in each state, whereas the Social Security Administration applies for Medicare.
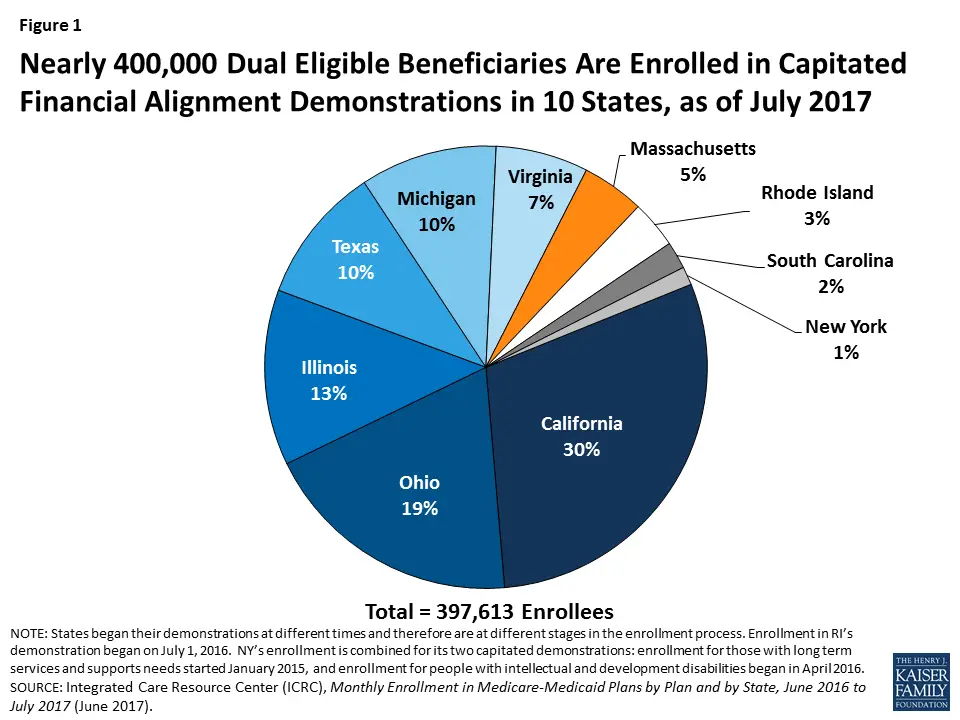
Profile Of The California Medicare Population
THE ISSUE
Understanding the characteristics of Californias growing Medicare population is important for the state and its stakeholders to understand the needs of these beneficiaries and identify opportunities to support them.
OUR WORK
ATI prepared this chartbook, Profile of the California Medicare Population, for the California Department of Health Care Services Office of Medicare Innovation and Integration with support from The SCAN Foundation. The chartbook highlights California Medicare beneficiary demographics including age, sex, race, and ethnicity. It includes analyses of Medicare Advantage enrollment and dual eligible beneficiaries both statewide and by county.
OUR VIEW
States have an opportunity to move upstream in the care of their residents, but it requires investment in understanding the needs of the broader Medicare population, including, but not limited, to dual eligible beneficiaries. OMII is the first dedicated Medicare office within a state Medicaid agency focused on strategic research and program design for Medicare and dual eligible state residents. ATI is honored to be a part of the team supporting OMII as it lays the foundation for future work.
This first chartbook is intended to help stakeholders and policymakers understand the characteristics of beneficiaries, what programs they are enrolled in, and where they live, all to inform the development of policies and programs to best serve this population.
You May Like: Is Invisalign Covered By Medicaid
Option : Original Medicare
- Medicare is primary and Medi-Cal is secondary. In Original Medicare, also known as fee-for-service, it is important to present providers with both Medicare and Medi-Cal cards. With Original Medicare you can choose any medical provider that accepts Medicare and Medi-Cal, no referrals to a specialist is needed.
- In addition to the Medicare and Medi-Cal card, beneficiaries also have a CalOptima Member Identification card and a Part D Prescription Drug Plan card.
- Medi-Medi beneficiaries that do not enroll in a Part D Plan or a Medicare Advantage Plan will automatically be enrolled in a Part D benchmark plan. Medi-Medi beneficiaries are automatically eligible for , the program that helps pay for prescription drug plan co-payments.
Your Rights & Protections
- Medi/Medi beneficiaries should not be billed for Hospital & Medical Services, it may be improper billing
-
Make sure to check that your prescription drugs are covered under the plan
- There is a Special Enrollment Period for people receiving Extra Help or designated as Medi/Medi. Exception: Medi/Medis may join or leave OneCare Connect at any time
Recommended Reading: How Long Is A Child Eligible For Medicaid
Option : Medicare Advantage Plans
- Medicare Advantage Plans are a type of Medicare health plan offered by private companies that contract with Medicare to provide Part A and Part B benefits. Most Medicare Advantage Plans also offer prescription drug coverage.
- In Orange County, Medicare Advantage are either an HMO or PPO. Plan members are assigned a medical group and referrals are required prior to seeing a specialist. MA plans pay first, and Medi-Cal pays any remaining cost sharing amounts. Beneficiaries need only present their MA Plan card when obtaining medical services.
What Type Of Coverage Do You Get If You Are Dual Eligible For Medicare And Medicaid
There are two levels of coverage for beneficiaries who are dual eligible:
- Full dual eligibleFull dual eligible refers to those who receive full Medicaid benefits and are also enrolled in Medicare. People who are full dual eligible typically receive Supplemental Security Income benefits, which provide cash assistance for basic food and housing needs. Qualifying as full dual eligible is based on your assets, which include checking and savings accounts, stocks, real estate and vehicles .
- Partial dual eligiblePartial dual eligibility includes those who receive assistance from Medicaid in order to help pay for Medicare costs such as premiums, coinsurance or deductibles. Partial dual eligibles fall into one of four categories of eligibility for Medicare Savings Programs.
A Medicare Savings Program is a federally funded program administered within each state that helps lower income people pay for Medicare premiums, deductibles, copayments and coinsurance.
The four Medicare Savings Programs are outlined below.
Recommended Reading: Dental Surgeon That Accepts Medicaid
What Medicaid Helps Pay For
If you have Medicare and qualify for full Medicaid coverage:
- Your state will pay your Medicare Part B monthly premiums.
- Depending on the level of Medicaid you qualify for, your state might pay for:
- Your share of Medicare costs, like deductibles, coinsurance, and copayments.
- Part A premiums, if you have to pay a premium for that coverage.
Terms Of Use For 1 To 10 Individual Documents Upload
I have elected to upload a group of individual files by identifying and attaching up to 10 individual files. I understand that the files will be named based on the information I enter for each file and that the file name will identify the member that the care coordination document is/are associated with. Additionally, I understand the importance of ensuring that the file is/are named correctly. I certify that the files will be carefully audited and confirmed to be accurately named before confirming my upload. By confirming my upload, I am representing that the file is/are named accurately.
Also Check: Obgyn In Broward County That Accept Medicaid
Unitedhealthcare Senior Care Options Plan
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plans contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
People Who Have Both Medicare & Medicaid
People who have both Medicare and full Medicaid coverage are dually eligible. Medicare pays first when youre a dual eligible and you get Medicare-covered services. Medicaid pays last, after Medicare and any other health insurance you have.
You can still pick how you want to get your Medicare coverage: Original Medicare or Medicare Advantage . Check your Medicare coverage options.
If you choose to join a Medicare Advantage Plan, there are special plans for dual eligibles that make it easier for you to get the services you need, include Medicare coverage , and may also cost less, like:
- Special Needs Plans
- Medicare-Medicaid Plans
- Program of All-Inclusive Care for the Elderly plans can help certain people get care outside of a nursing home
Don’t Miss: Medicaid Health Insurance Income Limits
Qualified Medicare Beneficiary Program
This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments.
Eligibility requires:
- Income of no more than $1,094 per month for an individual in 2021, or $1,472 per month for a married couple
- Resources of no more than $7,970 for an individual in 2021, or $11,960 for a married couple
Can You Have Medicare And Medicaid At The Same Time
Medicare and Medicaid are both public health insurance programs. If you are dual eligible, you can have both Medicare and Medicaid coverage at the same time.
Two of the key differences between Medicare vs. Medicaid include:
- Medicare is for people age 65 and over and for certain people under 65 who have a qualifying disability. Medicare eligibility is consistent for everyone across the U.S., no matter what state you live in.
- Medicaid is for people of any age who meet certain income qualifications. Medicaid is administered by state governments, and eligibility requirements can differ between states.
Don’t Miss: West Virginia Medicaid Provider Enrollment
Learn About Plan Types
CA Medicaid, or Medi-Cal, is health insurance for people with low incomes. You might be able to get Medicaid in California if youre pregnant, have children or live with a disability. In some cases, other adults also may qualify. Costs to you are low and based on your ability to pay. Its important to know that Medicaid rules and coverage differ from state to state.
Dual Special Needs Plans are for people who get both Medi-Cal and Medicare. Dual plans cover doctor visits, hospital stays and prescription drugs. They offer more benefits and extras than Original Medicare. Youll keep all your Medi-Cal California Medicaid benefits too.
Looking for the federal governments Medicaid website? Look here at Medicaid.gov.
Detailed Reporting Expectations In T
The State Medicare Modernization Act Files of Dual Eligibles are considered to be reliable, current sources of information on the dual-eligible population. States submit these files monthly to CMS for purposes related to the administration of Medicare Part D benefits. Because the T-MSIS and MMA counts by dual code both count the same populations on a monthly basis, they are expected to be generally consistent. States can therefore consider these MMA files as a useful resource for validating dual code classifications in T-MSIS .
It is also important to remember the intent behind dual codes 08 and 09, which are broader dual categories, to ensure that they are being assigned correctly:
You May Like: Dermatologist In Montgomery Al That Accept Medicaid
% California Working Disabled Program
The 250% California Working Disabled program helps Californians who are working, disabled and have income too high to qualify for free Medi-Cal. Californians who qualify may be able to receive Medi-Cal by paying a small monthly premium based on their income. Premiums range from $20 to $250 per month for an individual or from $30 to $375 for a couple.
To qualify, you must:
Also learn about how AB 1269 made the California Working Disabled program event better. This bill was signed into law in 2009 and became effective August 2011.
All these CWD rules are explained in more detail in the Medi-Cal section of the Disability Benefits 101 website.
Qualified Medicare Beneficiary Or Qmb
The QMB program assists beneficiaries in paying Medicare Part A and Part B monthly payments, coinsurance, and deductibles. As a general rule, the income limit is set at 100% of the Federal Poverty Level plus a $20 allowance. This means that a single candidate can earn up to $1,093 per month, and a married couple can earn up to $1,472 per month. The asset thresholds are higher than those for full Medicaid coverage. A single applicants limit is $7,970, and a married couples limit is near $11,960.
Don’t Miss: Neurologist In Alexandria La That Accept Medicaid
Long Term Care Benefits
Medicaid offers a wide range of long-term medical care benefits and supports, allowing people to age in place or in their community. Medicare does not provide these services, but in 2019, some Medicare Advantage plans began offering a variety of long-term home and community-based benefits. Long-term care benefits may include the following. This is not a complete list, and not all advantages may be available in all states.
- Adult Day Health / Adult Day Care
- Assistance with Personal Care
- Transportation for Medical and Non-Medical Purposes
- Care During a Break
- Meal Delivery / Congregate Meals
Aged & Disabled Federal Poverty Level Program
If you are aged or disabled and are not eligible for the SSI program, you may be able to get Medi-Cal through the Aged & Disabled Federal Poverty Level program. To qualify, you must:
This Medi-Cal program uses SSI countable income rules as well as a few extra rules you should know. For more information, visit the Medi-Cal section of the Disability Benefits 101 website.
Don’t Miss: Montefiore Medicaid Office Bronx Ny
What Is Medicare Vs Medicaid
Medicare
An animated white speech bubble appears over an animated character’s yellow and blue head.
ON SCREEN TEXT: Medicaid 101
The speech bubble and character fall away. Blue text appears on a light blue background. White text appears in two animated circles below. The blue and green circles overlap.
ON SCREEN TEXT: Medicaid is a joint federal and state health program. Federal State
The text and circles fall away. Blue text appears surrounded by blue animated disks with dollar signs on them. Animated individual and family character graphics appear below the text.
ON SCREEN TEXT: It is for individuals, families and children with limited income & resources.
The text and graphics fall away. A white map of the continental U.S. appears on a light blue background. Green map marker icons dot the map. Blue text appears in the center of the map.
ON SCREEN TEXT: Each state creates its own Medicaid programs based on federal guidelines.
The map disappears. Blue text appears surrounded by animated green and white form and plus sign graphics.
ON SCREEN TEXT: Medicaid programs have mandatory benefits & optional benefits.
The text and graphics fall away. Blue text appears over an animated dark blue scale graphic. Yellow animated coins pile up on the left side of the scale and animated books pile up on the right side.
ON SCREEN TEXT: Medicaid costs will vary based on a person’s income and the state’s Medicaid rules.
ON SCREEN TEXT: Eligibility varies based on a state’s Medicaid rules.
Information For Nonparticipating Providers
The Department of Health Care Services , in conjunction with the Centers for Medicare and Medicaid Services , is launching a three-year demonstration to enroll beneficiaries who are covered by both Medicare and Medi-Cal into managed care health plans. Enrollment in the Duals Demonstration, now known as Cal MediConnect, begins no sooner than January 1, 2014. Health Net is participating in Cal MediConnect in Los Angeles and San Diego counties.
Health Net’s Dual Eligible program goal is to improve the quality of care its Medicare Advantage and Medi-Cal managed care members receive by providing access to seamless, integrated care. The key component of Health Net’s Dual Eligible program is to promote better care and improve alignment and coordination of MA and Medi-Cal benefits.
The information links on this page are designed to help nonparticipating providers and their staff become familiar with the Dual Eligible Demonstration and Health Net’s Dual Eligible program.
Providers who would like information regarding participating in Health Net’s network can contact Health Net’s Provider Network Management Department by telephone at 543-9178.
< Back
Also Check: Medicaid Fraud Statute Of Limitations
